

Since 2008, la Caixa has offered support to patients with advanced illnesses, as well as resources for their families and professionals.
15 years ago, the La Caixa Foundation created a Comprehensive Care Program for people with advanced diseases. Its primary goal is to meet the emotional, social and spiritual needs of patients approaching the end of their lives and their families. Also raise public awareness of the importance of compassionate care in situations of chronic illness and social vulnerability, as well as conduct research and train professionals and volunteers. The goal is that psychosocial and spiritual support at the end of life is a right for all people.
Since its launch in 2008, the program has benefited more than 650,000 people, both patients and their families.
In coordination with the palliative care strategy of the National Health System, the Foundation’s “la Caixa” program provides its services through 65 psychosocial care teams (EAPS), consisting of almost 300 doctors, psychologists, nurses, social workers, pastoral agents and volunteers. which operate in all autonomous communities.
The program helps improve both the psychological symptoms (anxiety, depression, discomfort, suffering and insomnia) and the social consequences of advanced illnesses (relationships with family or environment), as well as important aspects of human dignity, such as acceptance or a sense of peace. with yourself and with others.
Since its launch in 2008, thanks to agreements with the Ministry of Health and various health departments of local autonomous communities, the program has provided services to more than 650,000 people – 290,181 patients and 372,630 family members – both in health centers and in residential homes and houses.
Initiative backed by results
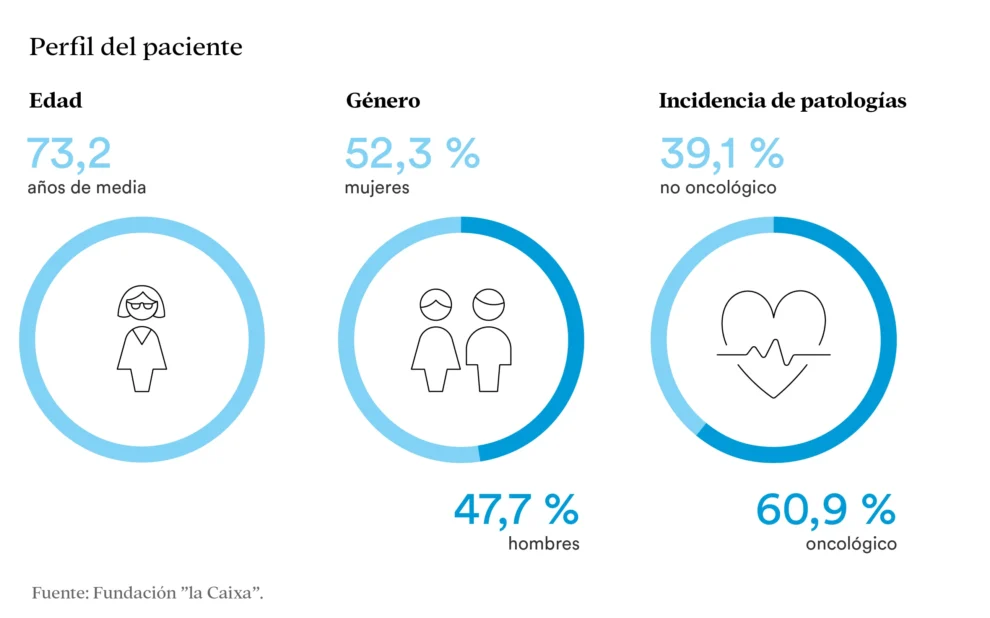
On October 14, to coincide with World Palliative Care Day, the La Caixa Foundation announced the results of the latest report on the effectiveness of the program. The assessment was developed in collaboration with the Department of Palliative Care of the University of Vic-Central Catalunya (UVIC/UCC) and the German Research Institute of Trias and Pujol (IGTP) on a sample of 6471 patients with advanced disease.
One of the main conclusions of the report is related to the improvement in the emotional state of patients. While 78% felt average or poor when they first attended EAPS groups, this percentage dropped to less than half after their intervention. The feeling of sadness also improved. Before psychosocial intervention, about 50% of patients felt very or very sad, but after receiving psychological, social and spiritual help, this percentage dropped to 17%. Moreover, 66% of service recipients believe that after participating in the Program, their beliefs and values help them cope with their situation.
“This assessment emphasizes the importance of a comprehensive approach: in disease situations, all aspects must be taken into account,” the doctor emphasizes. Xavier Gomez-BaptisteProfessor of Palliative Medicine and Scientific Director of the Comprehensive Care Program for People with Serious Illnesses of the La Caixa Foundation. “Our goal as professionals is to ensure that closure occurs in the best possible conditions and that care can be comprehensive in all cases, as all people deserve a peaceful and dignified end to life.”
Learn to live until the end
As part of its initiatives to disseminate the work carried out by the Program and the importance of comprehensive care for patients with advanced diseases, the La Caixa Foundation published an interview Gemma Nyerga with one of the professionals involved in this initiative. Near Ana Almanzapsychologist and leader of the psychosocial assistance team of the Red Cross of Almeria.
Almansa confirms that death is still a taboo topic, especially in situations of advanced disease. “We don’t make a habit of talking about it, and families often find it difficult to express their needs and fears in the face of a process that has no solution,” he explains. But “the end of life doesn’t have to be a difficult situation.” Even when there is no treatment, care remains.
According to Almanza, it is necessary to “break the pact of silence,” talk about the disease and “try to get the patient to show us what he needs to say and make the decision to end his life.” You must also be prepared for grief. And say goodbye. “Farewells are very important. When you accompany a patient and a family, there is rarely a complicated grief. This brings us to the essence of accompanying, listening, granting wishes so that there is no pain. It is so important to peace to those who leave and to those who remain.”
School of Educators
Unfortunately, we often distance ourselves from people who suffer from such situations. “And this is what we as a society must learn,” Almanza emphasizes: accompanying people to ensure they have a “serene and dignified end.”
Therefore, an important part of the Program is the School of Nurses. La Caixa Foundation offers a monographic series of workshops, in person or virtually, for informal caregivers and volunteers, led by experts in the fields of psychology, nursing, physiotherapy and social work. Structured in three areas –Know (technical content), Be (principles, values and emotions) and Do (Resources, Tools and Skills) – Workshops cover topics such as self-awareness, emotional support and compassion, coping with grief, nutrition or creative approaches to end-of-life care.
Seminars are offered in both face-to-face and virtual versions, have a maximum duration of two hours and are designed for a minimum of 10 and a maximum of 15 people. Those interested can write to [email protected] or call 900 223 040 from Monday to Friday from 9:00 to 17:00.
“We almost always die as we live. If we live peacefully, we die peacefully,” Almanza reflects, drawing on his daily experiences with late-life patients and their families. His advice on how to live the end of life well, both for yourself and for those around you, is to “be calm in the way we live, calm in making plans, calm in dealing with daily life. Express your needs, leave everything as it is.” explained that others can also be calm.
Source: El Independiente