
resistant bacteria.
Antibiotics have become humanity’s great allies in the fight against disease, and are cheap and readily available medicines for health systems. But we are so accustomed to them that bacteria develop resistance. This is what World Health Organization (WHO) calls the pandemic a silent one and estimates that by 2050 it could cost the lives of 10 million people. Just as quiet, according to the study cofares A third of the Spanish population (32.1%) do not know what antibiotic resistance is.
“That seems to be a very alarming number,” he muses. Rafael Canton of the Scientific Committee on COVID-19 and Emerging Pathogens of the College of Physicians of Madrid. “The survey that was made in 2019 included 1,270,000 people, and projections that over time will be close to these projections of 10 million people. It is estimated that there were 4,000 in Spain.”
This does not seem like a very high number, especially after the statistical insensitivity that the Covid death rate has caused us, but it is more than double the 1,700 people who died in traffic accidents. The figure could be much higher, but there is no consensus on how to measure cases.
The logical way out of this situation is the creation of new antibiotics, which has not happened since 1987. list of pathogens, priority for research. “Some of them are in the experimental stage, so they will appear,” Canton says. “It is desirable to extend the life of those that we have now, and when new ones appear, not to make the same mistakes as with the previous ones.”
To resolve this situation, European Commission works within a legislative framework that promotes the study of essential antibiotics. But the leaked draft proposal did not sit well with civil society or some European countries. The project is dedicated to the creation of transferable exclusive bonds.
The use of new antibiotics, when they appear, will not be massive, that is, those who invest in these drugs will not earn as much money as if they directed these resources to other drugs. The reason is that new antibiotics are prescribed when existing ones don’t work, they don’t reach many people, and the idea is that there is no abuse of consumption to create new resistance.
“Given the pharmaceutical industry’s lack of commercial interest in antibiotic R&D because it does not offer a large and attractive market, academic groups and small companies bear the brunt of antibiotic R&D,” Explain Jaime Manzano, Researcher at Health by Law.
- WHO list of priority pathogens for R&D of new antibiotics
- Priority 1: CRITICAL
- Acinetobacter baumannii, resistant to carbapenems.
- Pseudomonas aeruginosaresistant to carbapenems.
- enterobacteriaresistant to carbapenems, ESBL producers.
- Priority 2: HIGH
- fecal enterococcusvancomycin resistant.
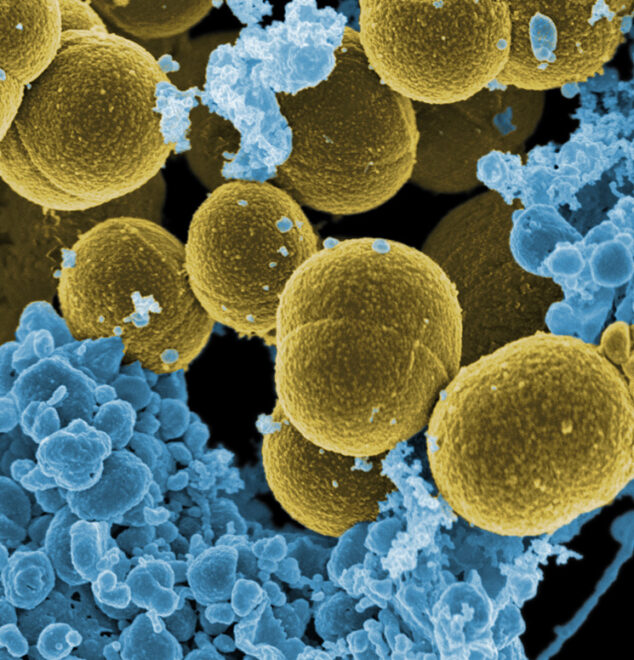
- Staphylococcus aureusresistant to methicillin, with intermediate sensitivity and resistance to vancomycin.
- Helicobacter pyloriresistant to clarithromycin.
- Campylobacter spp.resistant to fluoroquinolones.
- salmonellaresistant to fluoroquinolones.
- gonococcal neisseriaresistant to cephalosporins, resistant to fluoroquinolones.
- Priority 3: MEDIUM
- Pneumococcusnot sensitive to penicillin.
- Haemophilus influenzaeresistant to ampicillin.
- types of shigella.., resistant to fluoroquinolones.
“The bonus offer would be to give a company that brings a new antibiotic to market an extension of the exclusivity period for another product from the same company, or it could sell that right to another company so it can use it for its own purposes. product portfolio,” explains Manzano.
This means that whoever researches antibiotics will get some kind of prize so that the company can maintain a monopoly on a drug already on the market. A company develops an antibiotic and can sell this valuable bonus to another company that has a drug that sells in large quantities, such as cancer, whose patent is expiring and is about to lose its exclusivity. monopoly.
“Instead of finding a solution to the lack of innovative antibiotics, the voucher offer is slipping into a model based on monopoly markets that have failed to introduce a new class of antibiotics since 1987. Fourteen countries, led by the Netherlands, showed their opposition to the idea of bonds in a non-paper,” says Manzano.
According to this researcher, solutions “should be coordinated and inclusive from the beginning to the end of the innovation chain, with guarantees in public funding, and where global access, rational use and transparency of R&D costs are cornerstones. ”
Solutions to shortages and scarcity go through full transparency
Jaime Manzano
Darkness and Scarcity
The lack of transparency about the cost of medicines is part of the emerging shortage of medicines in the market. “The market and the commercial strategy of pharmaceutical companies are also often behind the scarcity. Medicines with lower prices or less profitable for companies tend to have more supply problems. In this sense, pharmaceutical companies often voluntarily withdraw certain medicines from the market in order to put pressure on the authorities in price negotiations or to facilitate the entry of other products of greater commercial interest to the company. These strategies particularly affect some essential medicines, such as generics for cancer or antibiotics,” the OCU says.
In the case of antibiotics, Rafael Canton argues that “the price of a drug is so low that it almost does not compensate when you think about what production is, the factors that determine the production of a substance in the field of biosecurity, packaging, transportation, etc. In the end, the final the price paid by neither the patient nor the state system does not compensate.”
The vast majority of current supply issues do not affect the patient
farmindustry
The pharmaceutical industry claims that “the vast majority of current supply issues do not affect the patient because therapeutic alternatives exist and furthermore because all pharmaceutical companies have contingency plans in place to avoid such issues, which include higher safety stocks. ‘ than at other times. precisely because of the multiplicity of factors affecting the world market and, especially, the European one.
“In recent years, there has been an increase in drug shortages in the EU, which indicates the need for the adoption of European pharmaceutical regulations to address their shortcomings in this regard,” emphasizes researcher Salud Por Derecho, who demands greater control over companies. . “Dealing with shortages and shortages includes full transparency about their exact causes, as well as the cost of this drug, to monitor situations in which it is alleged that the price does not allow for a reasonable benefit. In addition, there is a need to strengthen obligations for immediate notification of shortages and the risk of shortages, including longer notice periods in the event of a recall for commercial reasons, the obligation to maintain safety margins for medicines of high therapeutic value, and the imposition of sanctions in case of non-compliance”, he adds.
Source: El Independiente